
So, a viral pandemic has happened – the United States, along with the rest of the world, has had to take extreme measures to prevent the spread of a potentially deadly pathogen within our population. As it happens, this virus, also known as COVID-19, is particularly deadly to older adults and those with chronic medical conditions:
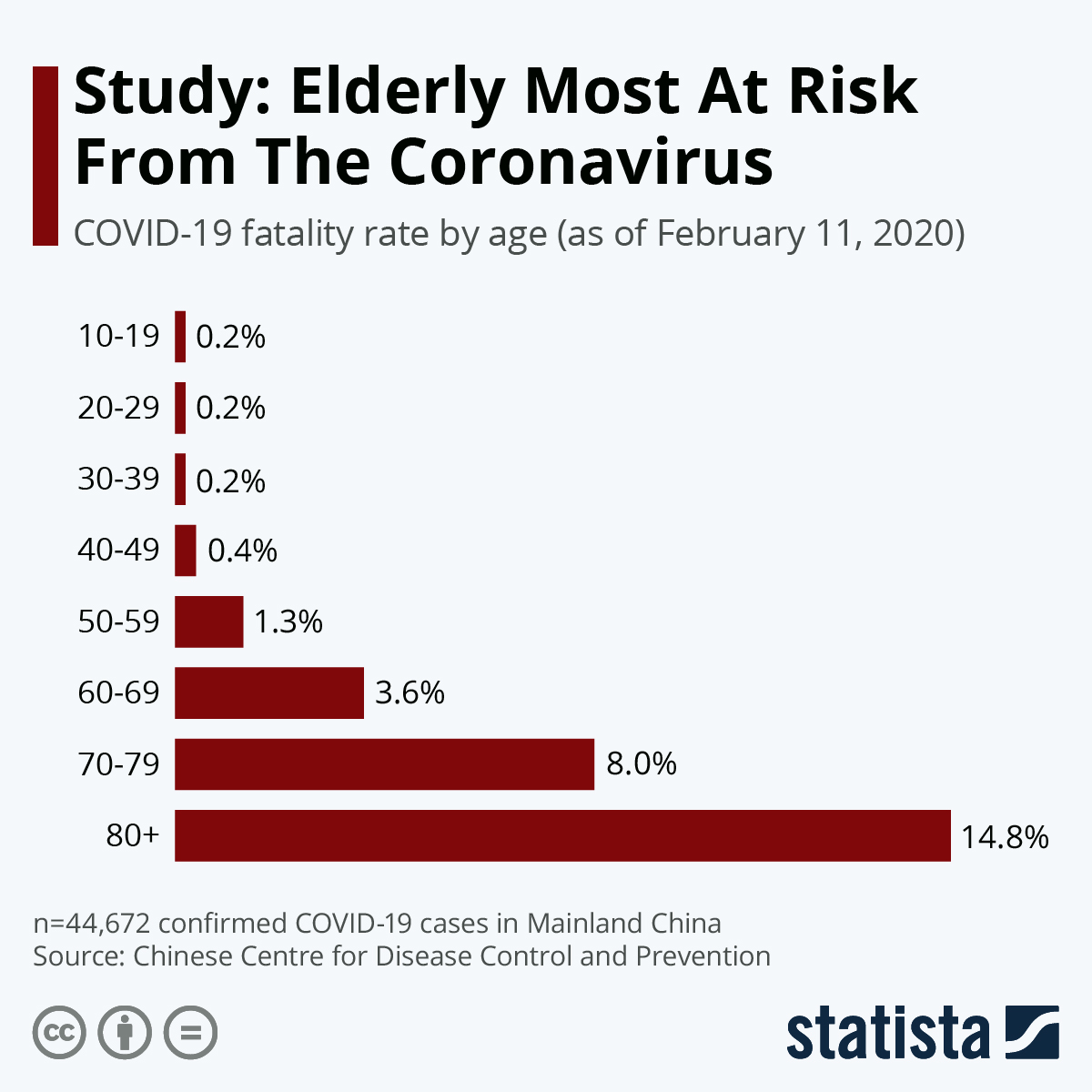
In response to this elevated threat to the older adult population, it’s now become the accepted advice that older adults should practice the most extreme forms of social distancing possible – with the US Federal Government’s Centers for Disease Control advising early on that older adults should “stay home as much as possible” and across the pond, in the UK, over-70s (all over-70s) will be subject to a mandatory quarantine for at least 4 months.

For us at Psychologists in Long-Term Care, this has highlighted something we have all known for quite some time – that older adults have, up until now only limited options for seeking mental health care when they are homebound and isolated. You would think that telehealth and telemedicine would have long been able to successfully fill the gap here – but not so fast. While older adults are quickly becoming tech-savvy and comfortable with technology, regulatory and bureaucratic limitations have held things back.
In my own personal blog and in a previous PLTC article by our esteemed former PLTC Treasurer, Alan Duretz in our Winter/Spring 2017 Newsletter (“CMS and Telehealth Reimbursement”), it’s been noted that while Medicare has in theory reimbursed psychological service providers for their services (psychotherapy, primarily) that are delivered via remote technology (so-called “e-therapy,”) in practice the regulations and limitations placed on these services have been so exacting that few, if any, providers have ever taken advantage of them. The main barriers have been the following:
- Requirement that e-therapy providers need use HIPAA compliant technology with “asynchronous store and forward” capabilities.
- Requirement that e-therapy is conducted in an audiovisual modality – e.g., telephone-only services don’t count.
- Requires that e-therapy consumers need to be located in an HPSA, or federally-designated Health Professional Shortage area
- Requires that e-therapy consumers receive services at an “eligible originating site” (e.g., typically a clinic or similar healthcare facility
- Requires that e-therapy services be provided to patients with whom you have a preexisting doctor-patient relationship (e.g., can only be provided to patients whom you have filed Medicare claims for over the last three years).
Something extremely noteworthy and groundbreaking is happening in the geropsychology and long-term care space in the midst of the COVID-19 crisis. Recently, at a press conference in Washington DC, Medicare administrator Seema Varna, flanked by President Donald Trump, Vice President Pence, and several other high-ranking officials, announced that they are relaxing #1, #3 #4, and #5 above (we’ll come back to #2 in a second).
In other words, this means that now, as long as psychologists make a “good faith” attempt to safeguard the privacy of their patients, they can now use platforms like Skype or Facetime to see older adult patients, and not be concerned about violating the HIPAA Privacy lsw. . There is a useful FAQ that was just released by CMS (Centers for Medicare Services) that you can read here. Moreover, these can be for newly-referred patients and residents in need, and therapy can be delivered in residents homes (whether the home is a facility or otherwise).
There’s a couple of catches, though. The waiver, known as “1135,” does not waive the requirement that providers use audiovisual modality with their patients. So, for the time being, telephone therapy is still not covered (except possibly in Texas or other states, see here). Which is unfortunate, because there are still any number of older adults out there who remain uncomfortable with videoconferencing and/or have visual limitations. Another is that the new waiver doesn’t spell out where providers can practice, so it’s not completely clear whether it’s acceptable for providers to deliver services from home, their office, or what have you (apparently APA has reached out to CMS to clarify this, and is awaiting a response).
So far, though, this is good – and really needed as the country tries to work through the COVID-19 crisis. But to me and others in PLTC – if rules and restrictions like these are to be relaxed during a crisis, it’s reasonable to ask whether these rules were necessary in the first place. COVID-19 will pass, but the problem of older adults being isolated and functionally impaired and unable to easily attend in-person medical or mental health appointments will remain, and technology is available to address these problems. Think about that.
Also, if you have anything to share about COVID-19 or how practice with older adults is changing in the face of this pandemic, please comment on this article below.
Finally, if you are a psychologist who practices in long-term care, or work with older adults in your practice and would like to learn more, we have an active Listserv, Newsletter, and other resources. Please consider joining PLTC:
http://www.pltcweb.org/membership.php#benefits
References / Links
APA PracticeUpdate on Telehealth
https://www.apaservices.org/practice/legal/technology/covid-19-telehealth-waiver
CMS FAQ on Waiver 1135
https://edit.cms.gov/files/document/medicare-telehealth-frequently-asked-questions-faqs-31720.pdf
Press Release from CMS
Summary of law specifying waiver (bottom section):
https://www.congress.gov/bill/116th-congress/house-bill/6074
